When an area of the brain experiences a sudden loss of blood, the event is called a stroke or cerebrovascular accident. Accompanying this circumstance is a loss of neurologic function. Strokes are broadly classified as either hemorrhagic or ischemic. An acute ischemic stroke refers to strokes caused by thrombosis or embolism and accounts for 85% of all strokes.
Extracranial embolism or intracranial thromboses are the most common cause of ischemic strokes. However, they may also be caused by decreases in cerebral blood flow—any process that disrupts blood flow can unleash an ischemic cascade. This leads to the death of neurons and cerebral infarction.
The emboli may arise from the heart or the extracranial arteries. However, they may also come from right-sided circulation (paradoxical emboli). Valvular thrombi may be caused by mitral stenosis, endocarditis, or prosthetic valves. Cardiogenic emboli other than valvular thrombi also include mural thrombi i.e. those created by myocardial infarction, atrial fibrillation, dilated cardiomyopathy, severe congestive heart failure, and atrial myxomas.
Thrombotic strokes can be divided into large vessel or small vessel strokes. Large vessel strokes include the carotid artery system; small vessel strokes include the intracerebral arteries (which includes the branches of the Circle of Willis and the posterior circulation.)
The most common sites of thrombotic occlusion are cerebral artery branch points. Arterial stenosis producing turbulent blood flow, atherosclerosis producing ulcerated plaques, and platelet adherence producing formation of blood clots that either embolize or occlude the artery are the events that cause pathology.
Within seconds to minutes of a decrease in blood flow, an ischemic cascade is unleashed. As ATP is depleted and membrane ion-transport systems fail, the ischemic neuron becomes depolarized. Substances released by the depolarized neuron then accelerate depolarization in other neurons—and the process cascades. Preservation of the area of oligemia in the ischemic penumbra is the primary goal of ischemia.
As noted in national guidelines, rapid recognition and diagnosis of intracranial hemorrhage (ICH) are essential to intervene in the frequently rapid progression from a sudden focal neurological deficit to a more generalized, fixed abnormality. This occurs progression occurs over a matter of hours.
Headache is more common with ICH than with an ischemic stroke and less common than in subarachnoid hemorrhage. Vomiting is more common with ICH than with either an ischemic stroke or a subarachnoid hemorrhage. Increased blood pressure and impaired level of consciousness are common.
History adds to the overall clinical picture and the patient—if possible—or witnesses should be questioned about trauma; hypertension; prior ischemic stroke, diabetes mellitus, smoking, use of alcohol and prescription, over-the counter or recreational drugs such as cocaine; use of warfarin and aspirin or other antithrombotic therapy; and hematological disorders or other medical disorders that predispose to bleeding such as severe liver disease.
Neurological examination is hugely variable with strokes—totally contingent upon the area of ischemia or bleed. Clinical loss of function does offer some idea of where the lesion is, but often a general state of neurologic shock will distort any meaningful assessment.
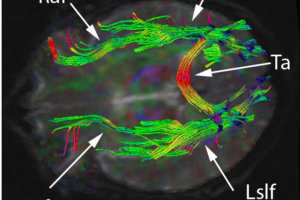
Brain imaging is obviously an important part of an initial evaluation. Computed tomography (CT) and magnetic resonance scans (MRI) are both able to identify an acute ICH as well as its size, location and hematoma production. CT may be somewhat better at visualizing demonstrating ventricular extension. MRI is superior at visualizing structural lesions and the amount of perihematomal edema and herniation. A CT scan with contrast may identify an associated aneurysm, arteriovenous malformation, or tumor.
Subarachnoid hemorrhage, abnormal calcifications, obvious vascular abnormalities, and blood in unusual locations, such as the sylvian fissure are indications for catheter angiography. Angiography may also be indicated in patients with no obvious cause of bleeding, such as those subjects with isolated IVH.
In animal models, thrombolytic therapy for acute ischemic stroke indicate that thrombolytic therapy administered within the first hour after stroke onset provides the greatest chance for success and effectiveness of thrombolysis beyond three hours after onset of ischemia in animals is minimal. There are only two studies that indicate a benefit with t-PA. t-PA is effective only if given within three hours of onset to appropriately selected patients.
Intracerebral hemorrhage is the major risk when using t-PA with a 6.4% rate of occurrence (0.6% in placebos.) 75 % of patients with a symptomatic intracerebral bleed were dead at 3 months.
This would appear to make t-PA an “undeal” as one researcher described it. However, even considering the increased mortality from intracerebral bleeds, the mortality of t-PA patients at 3 months was 17% while the increase in placebo treated patients was 21%.The implication is that most patients who had intracerebral bleeds had large strokes and would have died anyway, and patients with small strokes are less likely to die if treated with t-PA.
Thus, the use of t-PA has become a standard of care, if used, and if used in smaller strokes.
The problem with this recommendation is that it creates an impossible mandate on health care systems to not only diagnose a stroke but also determine the size of a stroke within three hours. An unbelievable amount of resources are now being devoted to evaluating how this can be done.
There have also been significant inroads been made in the recovery phase of strokes. These have been fitted into national guidelines that have formed the basis of standardization of care.