Along with vestibular neuronitis (VN) and benign paroxysmal positional neuronitis (BPPV), Meniere’s disease (MD) accounts for a majority of the cases of true vertigo seen by primary care providers. For considerable time, there was debate as to the pathophysiology associated with MD. It now appears that the constant pathological finding associated with its presence is progressive distension of the endolymphatic space of the inner ear. Thus, a synonym for MD is now endolymphatic hydrops.
It should be known that there is a distinction between Meniere’s disease and Meniere’s syndrome. Meniere’s syndrome refers to endolymphatic hydrops caused by a specific condition such as thyroid hormone disease or syphilis. Ménière’s disease refers to idiopathic endolymphatic hydrops.
The physical distention of the endolymphatic space damages both the hair cells of the cochlea and the organ of Corti. A distortion of the basilar membrane and the inner and outer hair cells are what cause hearing loss and tinnitus, and because the apex of the cochlea is wound much tighter than the base, hydrops affects the low frequencies located at the apex more than high frequencies.
Originally, MD was described as needing a triad of clinical symptoms—episodic vertigo, tinnitus, and hearing loss—to meet the criteria for diagnosis. Given the pathophysiology of the disease, progressive damage to the hair cells of the inner ear because of pressure from hydrops, it would seem that there should be a host of other symptoms. And indeed there are.
A prodrome of fullness or a blocked sensation in one ear is very common. Tinnitus is usually the next symptom, but vertigo follows shortly thereafter. Once the vertigo begins, it may last for hours or days. Nausea, vomiting, diarrhea, pallor, and sweating may all accompany an acute attack. Hearing may return to normal after an attack, but repeated attacks will usually decrease its acuity. Headache and ataxia may persist for days following an acute episode. Some of the attacks may be severe enough to cause patients to collapse—an event known as a Tumarik crisis.
Physical examination of a patient with suspected MD should begin with a complete neurological exam, cardiovascular exam, and inspection of the head and neck. The neuro exam should focus closely on cranial nerves.
There are a number of vestibular maneuvers that can help elucidate vestibular pathology. Both the Nylen-Bárány maneuver and the Hallpike maneuver activate the vestibular system. In the Hallpike maneuver, a patient is rapidly moved from the seated to lying position with his or her head tipped below the horizontal plane, 45 degrees to the side, and with the affected side downwards. The patient’s response relative to symptoms and nystagmus should be noted. When observing nystagmus, whether it is horizontal or rotatory, its fatigability, and its extinction with repetition are all important factors. Whether or not there is a latent period between the completion of the maneuver and the onset of nystagmus and the length of the latent period are crucial.
The maneuvers should be repeated several times over a 5-10 minute period, providing the patient can tolerate the repetition. Whether or not the severity of the symptoms decreases with successive repetition should be noted.
The peripheral vestibular dysfunction of MD should a short latency between the change in position and the vertigo, nausea, and malaise symptoms, a latency of several seconds after the change in position and before the onset of nystagmus, and fatigue and habituation of nystagmus and the vertigo, nausea, and malaise symptoms with repeated maneuvers.
Central lesions will produce an immediate onset of nystagmus, vertigo, nausea, and malaise. In addition, they will not habituate.
Audiometry is important because BPPV will produce vestibular findings quite similar to MD. But, BPPV disease is not associated with progressive hearing loss, and this offers an initial simple means of distinguishing between the two diseases with a reasonable degree of accuracy. The “benign” nature of BPPV over time establishes that differential. It is obviously helpful to document present hearing acuity and subsequent fluctuations by administering multiple hearing tests.
Lab studies should include thyroid stimulating hormone (TSH), T4, and T3, glucose, sedimentation rate and antinuclear antibody, renal functions, CBC and platelet count, electrolytes, FTA- ABS, and allergy testing for allergy-mediated Ménière’s disease.
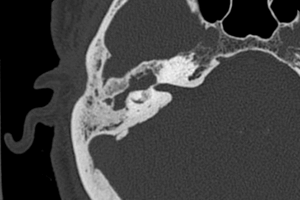
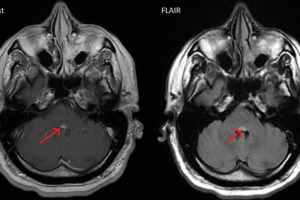
MRI and CT scanning are helpful to rule out acoustic neuromas or other cerebellopontine angle lesions, multiple sclerosis, Arnold-Chiari malformations, Dehiscent superior semicircular canals, and Widened cochlear and vestibular aqueducts.
Medical therapy utilizes medications that decrease symptoms, eg, meclizine [Antivert], droperidol [Inapsine], prochlorperazine [Compazine], diazepam [Valium], lorazepam [Ativan], alprazolam [Xanax]) mask the vertigo because they are vestibulosuppressants.
Diuretics such as hydrochlorothiazide and triamterene [Dyazide], hydrochlorothiazide [Aquazide], acetazolamide [Diamox], methazolamide [Neptazane]) have been used in an attempt to decrease fluid pressure in the inner ear and may help prevent attacks but are of little help after the attack is triggered.
Steroids can reverse vertigo, tinnitus, and hearing loss, probably by reducing endolymphatic pressure. The transtympanic administration of steroids is controversial, but it is gaining wider acceptance throughout the otologic community.
The ototoxicity of aminoglycosides has even been used to treat extremely severe MD. Such treatment leaves the patient with little or no balance function, and the resulting complete loss of inner ear function has been called Dandy syndrome.
A new device called the Meniett device is inserted via a tympanostomy tube and delivers pulses of pressure to the inner ear. Some patients have symptomatic relief when the device is used on a daily basis, but no long term studies have been performed.
In Europe, histamine agonists are also used.
Surgical treatment is reserved for those patients who have failed medical treatment. The procedures fall into the two general classes of destructive and non-destructive.