Bickerstaff brainstem encephalitis (BBE) is a rare inflammatory disorder involving the brainstem.
Clinical features of Bickerstaff Encephalitis
In a series of 62 patients with Bickerstaff Encephailitis there was a 3:2 male:female ratio.
The classic features of BBE include:
- Disturbance of consciousness, from drowsiness to the point of coma.
- Ophthalmoplegia, often presenting with diplopia.
- Ataxia, usually presenting as a gait disturbance with wide stance.
- Areflexia or hyper-reflexia (according to Odaka et al. patients without alterations in consciousness tend to be hyper-reflexic while those with alterations in consciousness are hyporeflexic or areflexic).
Additional features that can be found include:
- Pupillary abnormalities.
- Positive Babinski sign.
- Sensory changes including hemisensory loss or dysasthesia in one to four limbs.
- Facial diplegia.
- Nystagmus.
- Bulbar palsies including dysarthria.
- Belpharoptosis.
- Photophobia.
Limb weakness, when present in addition to disturbance of consciousness, ophthalmoplegia, ataxia and abnormal reflexes, suggests a diagnosis of BBE associated with GBS.
As is the case for many auto-immune disorders, BBE often follows a previous illness, most often an upper respiratory infection, by a few weeks.
Imaging characteristics of BBE
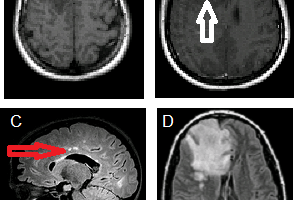
A review of 4 cases of patients with Bickerstaff Encephalitis by Berkowicz et al showed large, irregular hyperintense lesions on T2-weighted images in the midbrain, pons, and medulla. In one patient they also noted hyperintensity in the thalamus and cerbellar vermis. It should be noted, however, that most patients with BBE have no MRI findings: Odaka et al. report that only 30% of the 54 cases with MRI scans they reviewed had abnormalities on T2-weighted imaging in the brainstem or cerebellum.
Because pontine lesions without evidence of infection or vasculitis are also found with central pontine myelinolysis, rapid changes in osmolarity and serum sodium concentration should be ruled out.
Laboratory and electrophysiologic findings in Bickerstaff Brainstem Encephalitis
CSF can be normal or have albuminocytological dissociation. Odaka et al found that in the first week of presentation 19% of BBE patients had elevated protein relative to cell count, and the fraction increased to 57% three-to-four weeks after the onset of symptoms.
Anti-GQ1b antibodies are found were found in 66% of BBE cases, and onther ganglioside antibodies (anti-GM1, anti-GD1a or anti-GalNAc-GD1a) were found in 18% of cases
Differential diagnosis for BBE
Odaka et al. outline several disorders that should be excluded to make a diagnosis of BBE, these include:
- Miller Fischer Syndrome / Guillan Barre Syndrome (see next section)
- Vascular disease involving the brainstem
- Wernicke’s encephalopathy
- Multiple sclerosis
- Neuro-Behcet’s disease
- Botulism
- Myasthenia gravis
- Brainstem tumur
- Pituitary apoplexy
- Vasculitis
- Lymphoma
- Acute disseminated encephalomyelitis
Similarities and differences to other neurological disorders
There has been a long-standing debate as to whether Bickerstaff Brainstem Encephalitis is a distinct entity from Miller Fisher Syndrome (and to a lesser extent the general axonal variant of Guillain-Barre Syndrome). The similarities with Miller Fisher include brainstem lesions with ophthalmaplegia and other bulbar findings, as well as positive GQ1b antibodies.
Axonal loss on nerve conduction studies is consistent with the AMAN variant of Guillain-Barre syndrome. While many argue that BBE and GBS are separate entities, about half of BBE patients in Odaka et al.’s series had “BBE with overlapping GBS.”
The major differentiating features of BBE and MFS is that Bickerstaff has altered consciousness and can have abnormal Babinski reflexes, where as Miller Fisher does not.
Treatment for Bickerstaff Encephalitis
The primary therapy for BBE is removal of auto-antibodies either through administration of IVIg or through plasmapheresis. BBE is typically a monophasic disease with good recovery once the auto-antibodies are removed or neutralized.
Based on the similarity between BBE and GBS, Odaka et al recommend treating BBE with a combination of IVIg and high-dose methylprednisolone.
References
-
Odaka et al. (2003) Bickerstaff’s brainstem encephalitis: clinical features of 62 cases and a subgroup associated with Guillain–Barré syndrome. Brain 126:2279-2290. http://brain.oxfordjournals.org/content/126/10/2279.full
- Ogawara et al. (2002) Fisher syndrome or Bickerstaff brainstem encephalitis? Anti-GQ1b IgG antibody syndrome involving both the peripheral and central nervous systems. Muscle & Nerve 26:845-849. http://onlinelibrary.wiley.com/doi/10.1002/mus.v26:6/issuetoc
- Berkowicz et al. (2006) Bickerstaff’s brainstem encephalitis — an analysis of clinical and MRI findings. Neurol Neurochir Pol. 40:16-21.