Acute hearing loss can be secondary to a simple, common cause or can be what is considered a medical emergency. It is a circumstance that should be looked upon as serious until it has been reasonably well defined.
Acute primary hearing loss is called sudden hearing loss (SHL). It can be caused by viral and infectious causes, autoimmune causes, labyrinthine membrane rupture/traumatic, vascular etiologies, neurological diseases, and tumors.
Some its infectious causes are: meningococcal meningitis, rubella, mumps, mycoplasma, cryptococcus, all of the varicella viruses, and syphilis. Autoimmune inner ear disease (AIED) ulcerative colitis, lupus erythematosus, polyarteritis nodosa, and Wegener’s granulomatosis are autoimmune diseases that have been associated with SHK. Traumatic causes include perilymph fistula, inner ear decompression sickness, temporal bone fracture, inner ear concussion, otologic surgery (stapedectomy), and surgical complications of nonotologic surgery. SHL has been associated with the vascular conditions of vertebrobasilar insufficiency, sickle cell disease, and cardiopulmonary bypass. It has been associated with the neurological conditions of MS and migraine, and the tumors abd blood dyscrasias associated with SHL are acoustic neuroma, leukemia, myeloma, metastasis to internal auditory canal, and contralateral deafness after acoustic neuroma surgery.
Examinations of patients with SHL are usually normal. Still, a full neuro exam, including a Weber and Rinne, should be completed. Historically, patients should be specifically questioned about symptoms such as tinnitus, vertigo, dizziness, and aural fullness. They should also be questioned about previous ear surgery, ototoxic drug use, and recent URI symptoms. Specific attention should be given to trauma, loud noises, travel, airplane trips or trips to mountains, and other systemic diseases.
Statistically, roughly one-third of patients awaken with the hearing loss as well as vertigo.
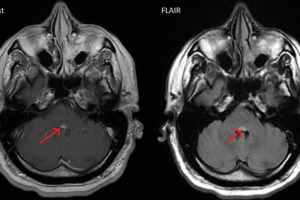
A reasonable lab workup would consist of a CBC, ESR, ANA titer, electrolyte panel, TSH, and biochem panel that includes cholesterol, triglycerides, and renal functions. Obviously, there will be a debate about whether or not an MRI is indicated. Unfortunately, this is a situation where logic indicates that an emergent MRI is not indicated since there are almost no conditions that require emergent intervention. That having been said, there is a consensus of opinion that audiology and MRI should be performed on all patients with a unilateral hearing loss.
Many treatments for idiopathic SHL have been tried but there is no standard accepted mode of therapy.
The simpler causes of sudden hearing loss are usually evident on a thorough otological exam. It is not uncommon for patients to develop an acutely plugged ear following a shower—even when they adamantly deny getting water in the affected ear. Impacted cerumen can trap small amounts of water or expand with increased humidity and completely occlude the external ear canal. This is usually evident on inspection with an otoscope.
A more classic history of cerumen impaction is of gradual, intermittent plugging and fullness.
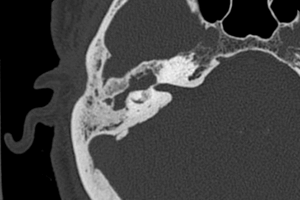
Trauma incurred during swimming and diving, blows to the external meatus of the ear canal, and even sudden decompression can cause a hemotympanum, resulting in hearing loss. Excessively loud noises can cause a concussive phenomenon that dislocates hair cells of the VIIIth nerve, also resulting in hearing loss.
The list of drugs associated with acute hearing loss is headed by the aminoglycosides— streptomycin, gentamycin, vancomycin, etc. Aspirin, caffeine, erythromycin, furosemide, methotrexate, chloroquine, and minocycline have also been implicated.
When hearing loss is secondary to a systemic illness, the systemic illness is usually expressed by other symptoms and is often acute and severe. Meningitis, stroke, etc. must be dealt with as a primary problem—hearing loss becoming of secondary concern.