The anterior middle and posterior cerebral arteries supply the majority of the cerebral cortex. However, thin regions of brain at the junction of these vascular territories are relatively under supplied by blood and especially sensitive to ischemia. These border zone regions occur in two patterns: cortical and internal border.
Cortical border zones include infarctions of the cortex and adjacent subcortical white matter in the frontoparietal lobes between the ACA and MCA territories and between the MCA and PCA territories in the parietal lobes. Internal border zone infarcts occur in the more inferior white matter of the corona radiata and centrum semiovale at the border between lenticulostriate perforators off the proximal MCA and penetrating cortical branches of the more distal MCA.
Diagnosis: Watershed infarct
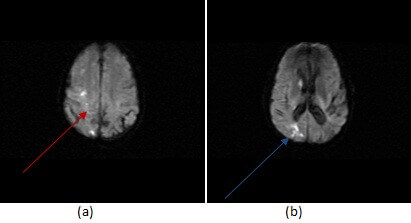
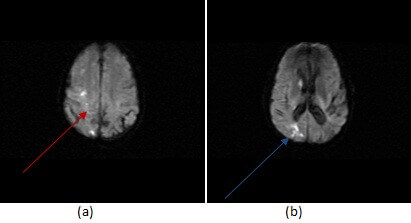
Figure 1: DWI imaging shows restricted diffusion in a watershed distribution between anterior and middle cerebral artery territories (a,red arrow) and between the ACA, MCA and PCA territories in the parietal lobe (b, blue arrow).
Watershed infarcts typically present as multiple small infarcts in the specific regions described above. These small infarct, aligned in a watershed territory, create a “rosary” pattern. Most watershed infarcts result from hypoperfusion to the cortex. This might be from cardiac arrest, severe ICA stenosis or medical causes of hypotension. When watershed infarcts are suspected, especially when unilateral, it is important to image the carotids (through ultrasound, MRA or CTA) to exclude the possibility of a treatable obstructing lesion.