Carotid/vertebral artery dissection is an underdiagnosed disease that can result in substantial morbidity. It has an incidence of 1-1.5/100000 and disproportionately affects young patients. Diagnosis is challenging clinically because the symptoms are often non specific and most commonly include unilateral headache and neck pain with more specific (but less sensitive) symptoms including Horner’s syndrome, cranial neuropathies and a neck bruit.
Diagnosis: Vertebral artery dissection on CTA
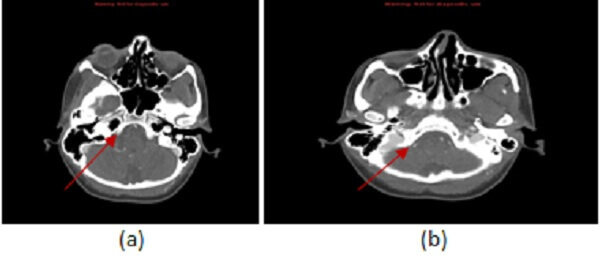
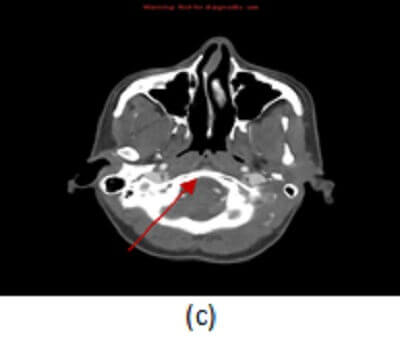
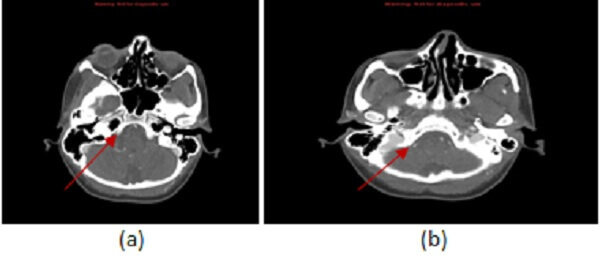
Figure 1: (a)-(c) Sequential axial images from a CT angiogram of the head and neck demonstrate an abrupt caliber change of the distal right V4 segment of the vertebral artery (red arrows) tapering in a “string” sign consistent with the diagnosis of dissection.
About 20% of the time dissection presents with ischemic stroke and this diagnosis should always be considered in the work up of an infarct in a young patient. In fact, dissection accounts for 20% of strokes in patients under 45. Dissection has a mortality of 4-8% and causes significant neurological sequelae in 14-24% cases. Aside from stroke, vertebral artery dissection may present with subarachnoid hemorrhage if the dissection involves the intracranial segment (V4) of the vertebral artery.
Dissection is most commonly due to trauma, occurring in about 1% of all trauma patients. Iantrogenic dissections can occur with cerebral angiography or Chiropractic manipulation (specific to the vertebrals). Spontaneous dissection may occur in patients with arterial wall disease e.g. fibromuscular dysplasia, marfans, ehlers danlos, polycystic kidney. Anticoagulation to prevent thromboembolic infarct is the treatment of choice in dissection.
Pathophysiologically, two types of dissection are recognized. Steno-occlusive dissection results when arterial blood enters the potential space between the innermost (intimal) and middle (media) layers of the vessel wall. The blood coalesces into a hematoma , which compresses the vessel wall causing a long tapered narrowing of the arterial lumen. The second form of dissection is a dissecting aneurysm. This results from blood tracking through the intima into the potential space between the media and adventitia leading to the formation of a aneurysm which lacks a true wall (pseudoaneurysm).
MRA and CTA are the most commonly used imaging modalities to evaluate for dissection. Imaging findings common to both modalities include: long segment smooth tapering of the vessel – “string sign”, vascular occlusion (absence of contrast or signal in the vessel lumen), focal lumen caliber change
and intimal flap with a double lumen for the steno-occlusive form; eccentric dilation of the vessel with luminal contour irregularity for the aneurismal form.
CTA is a sensitive modality to detect carotid and vertebral artery dissection. The typical protocol requires the injection of 65 cc of non ionic intravenous contrast at a higher rate (4 cc/sec) using a large bore (18 g anticubital) IV. Findings specific to dissection on CTA include a suboccipital rind, manifested by thickening of the vascular wall without caliber change, and an intramural hematoma, manifested by crescentic hyperdensity (since both blood and contrast are hyperdense on CT, this finding is better appreciated on non contrast sequences which are often done prior to the CTA).