The dural venous sinuses are responsible for draining blood and CSF from the brain. They include the superior and inferior sagittal sinus, straight, transverse, sigmoid and cavernous sinuses. Venous sinus thrombosis can be a life-threatening disease with allusive symptoms. Patient’s typically complain of headache with or without focal neurologic deficits.
Diagnosis: Dural venous sinus thrombosis
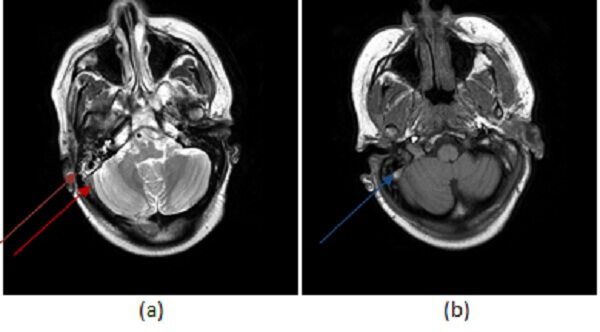
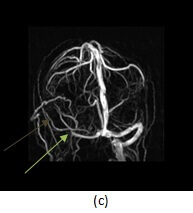
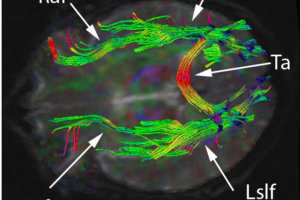
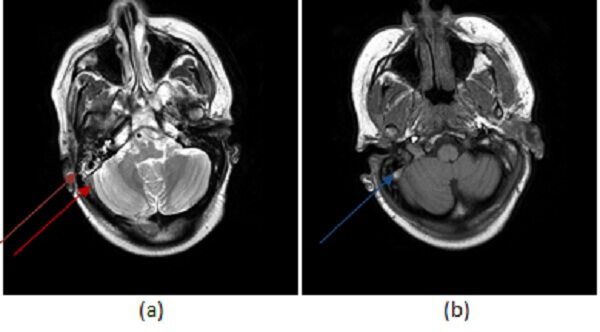
Figure 1: (a, red arrow) T2 and T1 (b,blue arrow) images demonstrate increased signal in the right sigmoid sinus. This finding could be due to either thrombosis or slow venous flow. There is also fluid in the mastoid air cells (purple arrow)- while fluid in the mastoid air cells is typically sterile, fluid can reflect infection in the case of mastoiditis, and mastoiditis predisposes to venous thrombosis.(c,green arrow) 3-D reconstructions from an MR venogram demonstrate abrupt cut off of contrast in the right transverse sinus with the suggestion of collateral flow (brown arrow) more consistent with thrombosis.
However, the spectrum of symptoms is broad ranging from none at all to coma and death. Women are at greater risk. Trauma, surgery, infection/inflammation, pregnancy, oral contraceptive use, dehydration and systemic disease such as coagulopathy (factor V Leiden) and collagen vascular disease place patients at greater risk for venous sinus thrombosis.
Diagnosis is typically made on imaging. It can be suggested on conventional MRI with abnormal signal in the venous sinuses. Typically, the sinuses should demonstrate dark flow voids on T1 and T2 imaging. On a given T1 or T2 sequence, the sinus may not be completely dark due to inflow effects, motion and other artifacts. However, persistent increased signal in the venous sinus on T1 and T2 imaging raises the question of an abnormality – either slow flow in the sinus or thrombosis.
If there is clinical or imaging suspicion for venous sinus thrombosis, a CT venogram or MR venogram should be performed. These studies provide better delineation of the sinuses and are typically performed with contrast. A common pitfall in the diagnosis is dural sinus thrombosis is the hypoplastic transverse sinus which can mimic occlusion. Thrombosis typically causes a frayed appearance to the venous sinus that may be associated with collaterals.
Large arachnoid granulations can also appear as filling defects within the sinus however, arachnoid granulations tend to be ovoid in shape while thrombosis tends to be long and linear. Arachnoid granulation should also have CSF signal intensity on MR and CT
Associated signs can also help differentiate venous sinus thrombosis from its mimics. Venous sinus thrombosis causes infarcts (either hemorrhagic or non-hemorrhagic) in about 50% of cases. There may be associated with cerebral edema and increased intracranial pressure. Dural arteriovenous fistulas can be a long term sequelae.
Treatment is through systemic anticoagulation. In rare circumstances for extensive thrombosis with symptoms, mechanical thrombectomy may be attempted by interventional neuroradiologists.