Dysautonomia occurs in about a quarter (10% to 35%) of traumatic brain injury patients. TBI dysautonomia is characterized by a varible combination of signs ymptoms including tachycardia, hypertension (or hypotension), muscle rigidity, extensor posturing, tachypnea, and diaphoresis.
Clinical presentation of TBI dysautonomia
TBI dysautonomia typically presents 1-2 weeks after severe brain injury, once ICU sedation has been discontinued. In a meta-review Baguley et al. (1999) found that on average tachycardia manifests about 10 days after injury, with an average heart rate around 120 bpm. Respiratory rate started to increase around day 7, with maximum rates around 25 breaths per minute on days 14-19. Temperature ran about 0.5 to 0.75 deg C higher than control patients throughout the hospital stay, and temperatures were already elevated at day 3.
The features of dysautonomia, even after treatment, often last 2-3 months after traumatic brain injury. Hendricks et al. reported duration of symptoms lasting anywhere from 3 to 68 days (mean 20.1 days). Patients with diffuse axonal injury are much more likely to have TBI dysautonomia, and on average their outcomes are significantly poorer with more frequent secondary complications.
Differential diagnosis
TBI dysautonomia is a diagnosis of exclusion, and several other syndromes have a similar presentation. These include:
Neuroleptic malignant syndrome: characterized by hyperthermia, muscle rigidity, delirium and autonomic instability, NMS can appear to be very similar as TBI dysautonomia. Unlike TBI dysautonomia, however, creatine phosphokinase is typically elevated in NMS. Because NMS is associated with recent initiation or dose changes in neuroleptics, if no neuroleptics have been used NMS is unlikely.
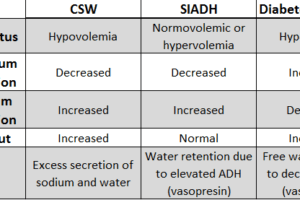
Thyroid storm: Thyroid function tests should be checked to rule out thyroid storm as an etiology for hyperthermia and tachycardia. This is particularly important in patients with neck injuries that could have traumatized the thyroid gland.
Malignant hyperthermia: Malignant hyperthermia should be ruled out in post-surgiclal patients anesthetized with volatile anesthetics or patients paralyzed with succinylcholine for mechanical ventilation.
Serotonin syndrome: Serotonin toxicity shares many features of TBI dysautonomia, including tachycardia, tachypnea, fever, and hyper-reflexia with clonus. It usually also has alterations in mental status including delirium, hallucinations, or even coma. Review of medications is imperative to identify those that would increase synaptic serotonin concentrations.
Treatment of traumatic brain injury dysautonomia
After ruling out other potential causes of dysautonomia, therapy should be directed at 1) maintaining normal core temperature (because control of cerebral perfusion is poorly regulated in dysautonomia, increased brain temperature can result in increased metabolic load without compensatory increase in blood flow, eventually causing ischemia and worsening brain injury), 2) reducing cardiac stress through control of hypertension and tachycardia with beta-blockers (propranolol is the first drug of choice, but other beta-blockers can be used), 3) control of tonic posturing with bromocriptine or dantrolene, 4) following “migraine criteria” to provide a low stimulus environment.
Contrary to previous protocols, new preliminary rehabilitation research suggests that morphine and ativan should be avoided as neurodepressants reduce neural plasticity needed for recovery (preliminary verbal report, RIC; this has not been validated in publications).
References
- Baguley IJ, Nicholls JL, Felmingham KL, Crooks J, Gurka JA, Wade LD Dysautonomia after traumatic brain injury: a forgotten syndrome? J Neurol Neurosurg Psychiatry. 1999 Jul;67(1):39-43.
- Hendricks HT, Heeren AH, Vos PE. Dysautonomia after severe traumatic brain injury. Eur J Neurol. 2010 Sep;17(9):1172-7. doi: 10.1111/j.1468-1331.2010.02989.x. Epub 2010 Mar 9.
- Baguley IJ, Cameron ID, Green AM, Slewa-Younan S, Marosszeky JE, Gurka JA. Pharmacological management of Dysautonomia following traumatic brain injury. Brain Inj. 2004 May;18(5):409-17.