A form of trans-cortical motor aphasia (TCMA), Supplementary Motor Area aphasia can occur in strokes of the Anterior Cerebral Artery (ACA) on the dominant hemisphere.
Most aphasias are the result of infarction of branches of the Middle Cerebral Artery, either affecting Broca’s area (Brodmann’s areas 44 and 45) or Wernicke’s area (Brodmann’s area 22). However aphasia can also develop in lesions of the ACA on the dominant hemisphere.

Image Caption: Supplementary motor cortex is shown in pink.
(Image by Paskari; Wikicommons license)
Supplementary Motor Area
The exact role of SMA is unclear, and most of the work trying to clarify its role has been done on somatic (rather than speech) motor functions in non-human primates. In the human, SMA was first described by Penfield and Welch (1951) as a motor representation of the body along the medial aspect of the cerebral hemisphere distinct from the primary motor cortex. Stimulation of the SMA can result in complex motor patterns, and it is sometimes thought of as contributing complex commands to the primary cortex that encodes more rudimentary motor commands to muscle groups (although there is significant controversy growing around this model).
The SMA is supplied in its entirety by the anterior cerebral artery (ACA). This distinguishes it from the primary motor cortex, which is supplied by the MCA on its lateral aspect (somatotopic face and arm regions) and the ACA along its medial aspect (somatotopic leg region).
The SMA has reciprocal connections with Broca’s areas, so is thought to contribute to motor control of speech patterns.
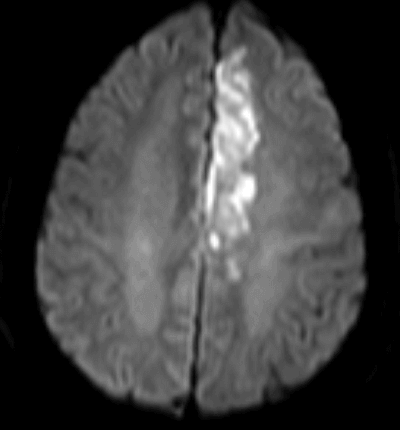
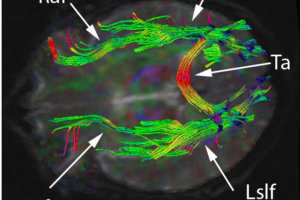
Image caption: Diffusion weighted MR image showing an acute ischemic infarct of the left ACA territory resulting in right leg weakness and an expressive aphasia with intact repetition.
Clinical characteristics of SMA aphasia
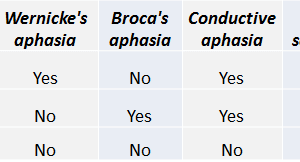
Freedman et al., 1984 describe the anatomical lesions of 15 cases of transcortical motor aphasia, and found that lesions of the ACA in the dominant hemisphere produced a clinically classic TCMA syndrome. The four criteria used by Freedman et al. to identify “classic TCMA” syndromes include limited spontaneous speech, intact repetition, normal articulation, and good auditory comprehension.Since the SMA sits in the ACA distribution, the aphasia that develops with an ACA infarct is attributed primarily to damage to the supplementary motor area (unlike other TCMA syndromes typically thought to be caused by hypoperfusion at the ACA/MCA watershed zone). This type of aphasia can present in the context of typical ACA findings, including: contralateral hemiparesis, with more paresis on the leg than arm, a tendency to look toward the side of the lesion, and a loss of spontaneity.
Lesions restricted to the left SMA (dominant hemisphere) produce an aphasia thought to be due to an inability to initiate language production, with little to no spontaneous speech (Freedman et al., 1984). Because Wernicke’s area and the arcuate fasciculus are intact, object naming, comprehension, and word repetition are intact. Patients can have difficulty with other spontaneous language functions like reading aloud or writing, but are often still able to copy written material (Freedman et al., 1984; Pai, 1999).
Larger lesions involving the operculum, head of the caudate, or motor strip of the face can cause other symptoms including articulation difficulty, or comprehension problems without directly affecting Wernicke’s or Broca’s areas.
While we are not aware of formal longitudinal studies, clinical lore is that recovery from SMA aphasia can be excellent.
References
- Penfield, W. and Welch, K (1951). “The supplementary motor area of the cerebral cortex: A clinical and experimental study”. Am. Med. Ass. Arch. Neurol. Psychiat. 66: 289–317.
- Freedman M, Alexander MP, Naeser MA. Anatomic basis of transcortical motor aphasia. Neurology. 1984 Apr;34(4):409-17.
- Pai MC. Supplementary motor area aphasia: a case report. Clin Neurol Neurosurg. 1999 Mar;101(1):29-32.