Trauma accounts for approximately 1 in 3 ER visits nationwide and is a major public health problem. It is the leading cause of death amongst youth and young adults and a major source of morbidity and lost productivity. There are two basic kinds of trauma – penetrating and non-penetrating head trauma.
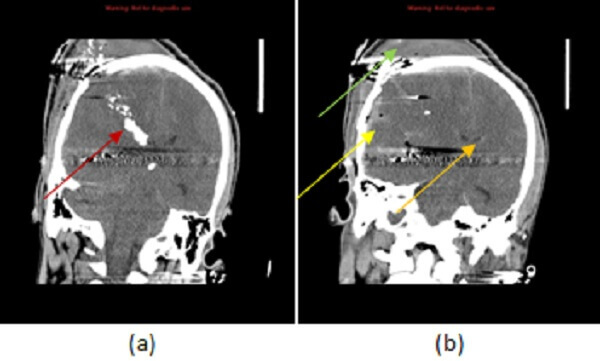
Diagnosis: Penetrating head trauma
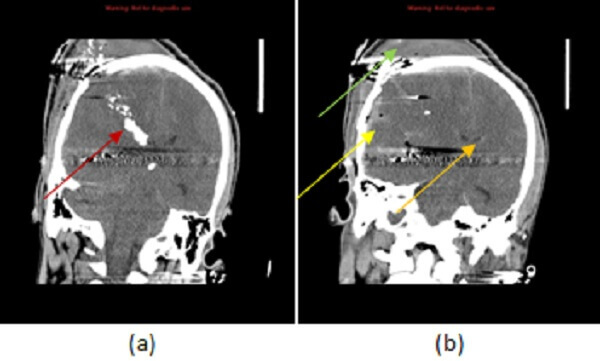
Figure 1: Unenhanced Head CT, Sequential images. (a) GSW with entrance wound in the high right parietal bone extending to the right ventricle (red arrow). Associated with traumatic subarachnoid hemorrhage, pneumocephalus (yellow arrow for both) and right to left midline shift (orange arrow Subgaleal hematoma (green arrow).
Penetrating trauma involves ballistics and causes approximately 50,000 fatalities/year – 60% from suicide and 40% from homicide. Gun Related Homicide is 2-4 times higher in the US than in other developed countries. While most GSW are non fatal (13:1), they cause substantial morbidity and lost productivity. Young (13-17) male minorities are particularly at risk.
When evaluating the imaging of a trauma patient in a comprehensive fashion, it is helpful to use a “3 T’s” search pattern: Terrible complications, tissues (primary damage) and other targets (secondary damage and delayed complications). Add a 4th T – trajectory for penetrating trauma. Terrible complications of head trauma include most of the indications for emergent surgery such as midline shift/subfalcine herniation greater than 10 mm, evidence for uncal or tonsillar herniation and large intracranial hemorrhage combined with a GCS of at least 5. The trajectory of the bullet is an important determinant of prognosis – trajectories with transhemispheric, transventricular and posterior fossa involvement confer a worse prognosis. Tissues include immediate consequences of trauma including hemorrhage – intraparenchymal and subarachnoid – pseudoaneurysm, comminuted depressed skull fractures (depressed fractures are more likely to be treated surgically) and increased intracranial pressure (manifested by effacement of the cerebral sulci and poor grey-white differentiation). Subgaleal hematoma (scalp soft tissue trauma) is commonly seen and can be an indication of the bullet trajectory or additional non penetrating trauma. Finally other targets include delayed complications of trauma such as hydrocephalus (from obstruction due to intraventricular hemorrhage), ventriculitis and infection (intracranial abscess, subdural empyema).