Trauma is the sixth leading cause of death world wide. Non-penetrating head trauma is the most common form of trauma and involves forces that impact but do not penetrate the parenchyma. Motor vehicle collisions and falls are the most common forms. Head injuries are a common consequence of nonpenetrating trauma, occurring approximately 30% of the time.
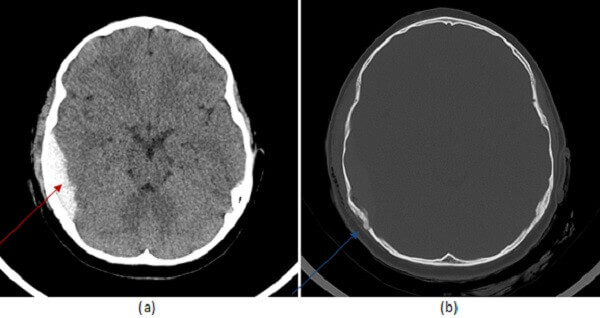
Diagnosis: Epidural Hematoma
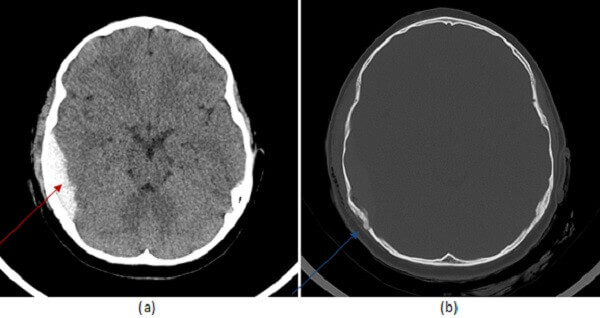
Figure 1: (a, red arrow) noncontrast head CT demonstrates a hyperdense extra-axial collection convex to the brain parenchyma which does not cross suture lines. It is associated with a fracture of the parietal calvarium (b, blue arrow).
The consequences of non penetrating neurotrauma can be conceptualized within a 3T framework – terrible complications, tissues, and other targets can be used to approach cases of nonpenetrating neurotrauma. Terrible complications are similar to penetrating trauma and include evidence of uncal or subfalcine or tonsillar herniation and/or midline shift. Brainstem herniation can sometimes be evidenced by a hemorrhage involving the ventral paramedian midbrain and/or pons, also called a duret hemorrhage.
Tissue consequences include the immediate sequela of trauma such as intraparenchymal, subdural, epidural or subarachnoid hemorrhage and cerebral edema.
Epidural hematomas are due to tears in the middle meningeal artery. They tend to be convex to the brain parenchyma, do not cross suture lines in the calvarium and may rapidly expand (under arterial pressure) sometimes in a delayed fashion resulting in a sudden neurologic decompensation hours after the trauma has occurred. By comparison, subdural hematomas are lentiform in shape and can cross suture lines. Subarachnoid hemorrhage occurs between pia and arachnoid layers and unlike subdural or epidural hemorrhage extends within the sulci of the brain parenchyma. It is important to look at the attenuation of the epidural hematoma, for epidurals with mixed density – the “swirl” sign- can be an indication of active or ongoing bleeding and bode a worse prognosis.