The third T in the 3T trauma framework (see cases on epidural hematoma and penetrating trauma) refers to “other targets” and concerns delayed complications of traumatic brain injury. These competitions include hydrocephalus, ventriculitis and diffuse axonal injury.
Diagnosis: Diffuse Axonal Injury
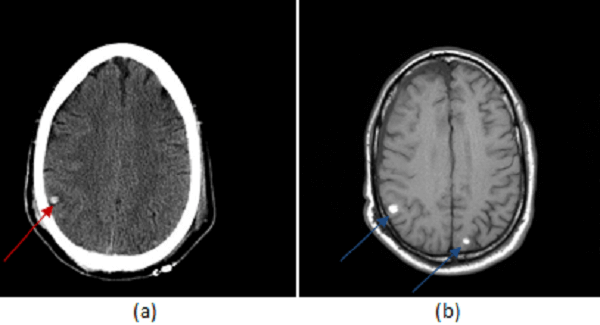
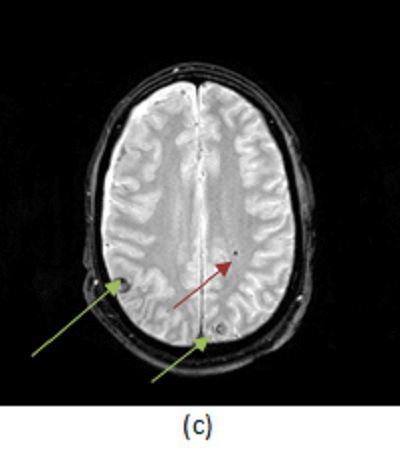
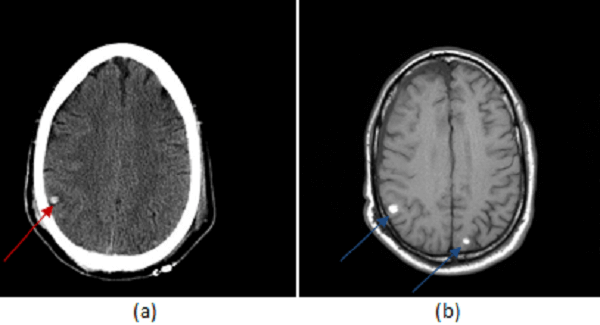
Figure 1: (a, red arrow) non contrast head CT shows a small hemorrhagic contusion in the right parietal lobe. (b, blue arrow) T1 weighted imaging demonstrates two small foci of T1 hyperintense signal consistent with hemorrhage at the grey white junction. (c, green arrow) T2* imaging is most sensitive for blood and intracranial trauma, demonstrating the hemorrhagic contusions identified in (a) and (b) but also a focus of diffuse axonal injury in the left frontal white matter (brown arrow). (Note the hemorrhages are INTRA-axial, not extra-axial as suggested by the answers.)
Diffuse axonal injury (DAI) is a long-term sequel of traumatic brain injury (TBI). It results from damage to axons induced by rapidly decelerations of the intracranial contents, as commonly occurs in trauma. The gray white junction is most susceptible and common locations include the corpus callosum, superior cerebellar peduncles, cortex, basal ganglia and thalamus.
On a microscopic level, diffuse axonal injury occurs because of secondary biochemical process initiated by the shearing injury, rather than direct mechanical injury. The chemical processes are poorly understood, but induce cytotoxic injury including increases in intracellular calcium with subsequent secondary messenger activation leading to disruption of the axon cytoskeleton.
Initial CT scans may be negative or demonstrate small hemorrhagic contusions. MRI is the gold standard for the evaluation of diffuse axonal injury and demonstrates foci of microscopic hemorrhage in susceptible areas. The appearance of blood on T1 and T2-weighted images depends on its age; these sequences are also less sensitive for the detection of small hemorrhagic foci. As such, susceptibility weighted (SWI) or gradient recalled echo (GRE, T2*) imaging is the preferred method for demonstrating axonal injury. Unlike T1/T2 (spin echo) imaging, SWI and GRE, are sensitive to local inhomogeneity in the magnetic field created by small amounts of blood or calcium – the result is that DAI manifests as a focal loss of signal on SWI or GRE as seen in Figure 1.
It is important to identify the presence of DAI because it has important prognostic implications. TBI dysautonomia, for example, most frequently occurs in the context of diffuse axonal injury.