The recent use of intravenous tissue plasminogen activator (TPA) to treat acute stoke has resulted in the introduction of “code strokes” in many emergency rooms, which typically require the coordinated efforts of the emergency room physician, the neurologist and the neuroradiologist . Since TPA can only be administered within a narrow window (around three hours) after the onset of symptoms, rapid evaluation is essential – hence the saying “time is brain”.
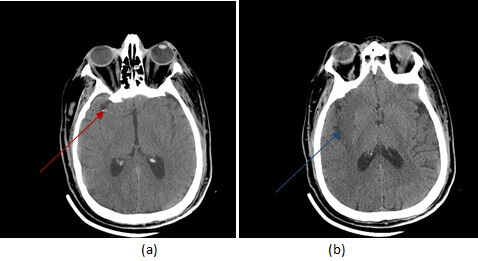
Diagnosis: Acute embolic non hemorrhagic right middle cerebral artery infarct on CT
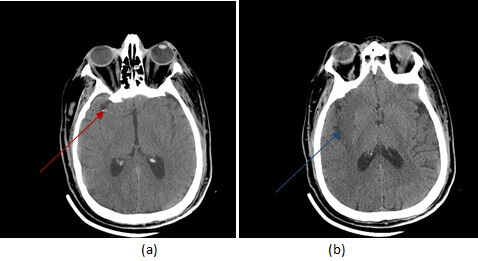
Figure 1: (a,red arrow) axial non contrast CT demonstrates a hyperdense middle cerebral artery. There is loss of grey white differentiation involving the insular cortex and right basal ganglia (b,blue arrow).
CT is the initial imaging modality performed in the code stroke protocol. It is done primarily to exclude a hemorrhagic infarct, an absolute contraindication to the administration of TPA. However CT can also suggest the presence of a non hemorrhagic infarct with a sensitivity of approximately 70% – blurring of the junction between grey and white matter, especially in the insula is an early and often subtle sign of a non hemorrhagic infarct. A hyperdense MCA reflecting the increased attenuation of an clot within the vessel , is a specific sign for an embolic infarct.
MRI is the gold standard for the diagnosis of stroke but is not typically performed during a stroke code because of time constraints- a CT that shows no hemorrhage and high clinical suspicion for stroke is enough to justify treatment. Of the MRI sequences, diffusion weighted imaging is by far the most sensitive.
Recognizing the CT signs of acute non hemorrhagic infarct is important in other situations as well. Patients who are poor historians, who have non specific clinical exams and “altered mental status” can all have stroke and CT is often the first imaging modality performed in these patients.