The most common cause for enlargement of the ventricles is ex vacuo dilation due to atrophy of the cerebral parenchyma. It is important to distinguish ex vacuo ventricular dilation from true enlargement of the ventricles (hydrocephalus).
Diagnosis: Normal pressure hydrocephalus (NPH)
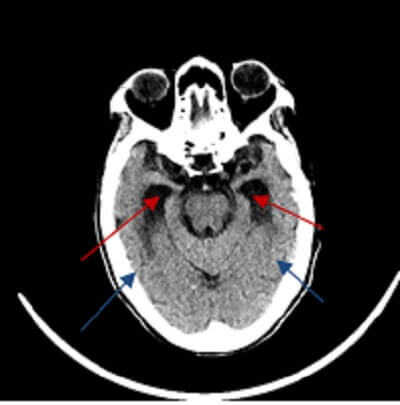
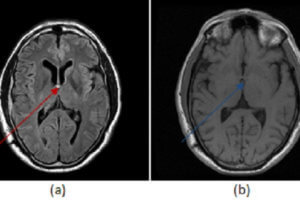
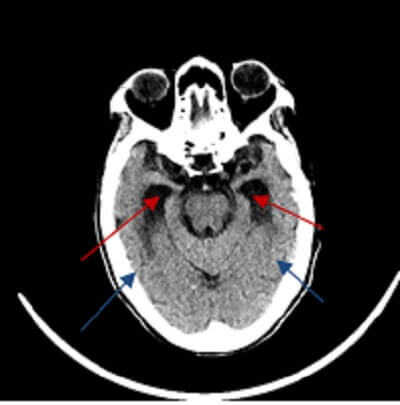
Figure 1: (red arrow) temporal horns of the ventricles are dilated out of proportion to sulcal atrophy, a finding suggestive of NPH.
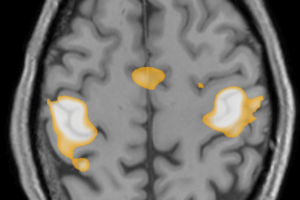
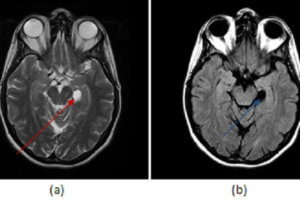
Imaging findings suggestive of hydrocephalus include enlargement of the temporal horns, convexity to the third ventricle with distention of the anterior recess and rounded corpus callosum, flattening and effacement of the sulci and transependymal fluid in the periventricular white matter (manifested by decreased attenuation on CT and increased T2 signal on MRI).
Hydrocephalus refers to enlargement of the ventricular system and two broad categories are recognized – communicating and noncommunicating.
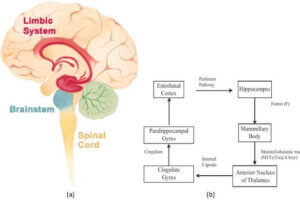
Communicating hydrocephalus results from microscopic obstruction of the arachnoid villi that drain CSF and blood into the venous system, such as from meningitis (chemical, infectious or neoplastic), surgery or subarachnoid hemorrhage.
NPH is a special form of communicating hydrocephalus and results from the disruption of CSF flow dynamics, possibly due to fibrosis of arachnoid granulations. About 50% are idiopathic and the other 50% are related to a secondary cause (meningitis, hemorrhage etc.). Unlike other forms of communicating hydrocephalus intraventricular pressure is not increased.
Distinguishing NPH from ex vacuo dilation of the ventricles is a difficult imaging problem as the conditions affect similar populations. NPH is suggested when ventricular dilation is out of proportion to the prominence of the sulci, but this is a subjective call. Transependymal flow of fluid around the ventricles and corpus callosal thinning suggest NPH, as does a flow void in the cerebral aqueduct (reflecting increased velocity of CSF).
NPH is important because it is a treatable cause of dementia and response to ventriculoperitoneal shunting. The best predictors of outcome to include aqueductal flow void , thinning of the corpus callosum, effacement of the sulci with absence of cortical atrophy and gait apraxia as the dominant clinical symptom.