Any symptoms that center on the head and neck are magnified by the fact that this is the most highly innervated part of the human body. Thus eye pain, ear pain, mouth pain are all tolerated to a lesser degree than extremity pain. It is also true that the amount of anxiety associated with these symptoms is greater.
The differential for facial numbness is diverse and lengthy. It includes demyelinating disease, trigeminal neuralgia, Bell’s palsy, stroke, inflammatory disease such as post viral neuritis, varicella zoster, neurofibromatosis, brain tumors, acoustic neuromas, sinus and middle dysfunctions including infection and barometric disease. Basically, follow the peripheral course of the fifth cranial nerve into the brain and then map the sensory connections to the rest of the brain and list the possible pathological influences on these anatomic areas. That creates a full differential diagnosis.
Trigeminal neuralgia is estimated to occur at a rate of 1.6 per thousand (internationally.) Its etiology continues to be an item that is debated. One theory proposes that peripheral injury increases afferent firing in the nerve. Another theory implicates a failure of central inhibitory mechanisms. Anatomically, an abnormal vascular course of the superior cerebellar artery, aneurysms, tumors, and chronic meningeal inflammation may all irritate trigeminal nerve roots. Patients present with pain that is brief and paroxysmal, characterized as stabbing or shocklike. It is usually severe. Its distribution, since this is a peripheral problem, is along one or more branches of the trigeminal nerve and is usually unilateral. It lasts for a few seconds, but continues throughout the day. The associated numbness will come on early in the disease and often not be recalled by patients when compared to the pain.
Bell’s palsy is primarily a muscular problem since it is a neuritis of the VIIth cranial nerve, but early on in its course, some numbness may be described.
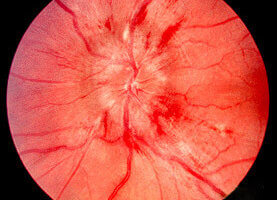
Demyelinating disease, multiple sclerosis (MS), can cause virtually any sensory deficit imaginable. MS is a demyelinization the CNS that typically presents with an variable combination of neurological as well as psychological dysfunctions. The disease may progress over years. A classic presentation for MS is involves the entities of optic neuritis, transverse myelitis, internuclear ophthalmoplegia, or paresthesias. Now MRI findings are also helpful in making the diagnosis. Typical findings on an MRI also help establish a diagnosis of MS. By convention, MS has been broken into the categories of definite, probable, or possible. Patients with an atypical presentation may also need evoked potential studies or cerebral spinal fluid studies to aid in the diagnosis.
MS appears to be an autoimmune disease with characteristic lesions described as multicentric, multiphasic CNS inflammation and demyelination.
With regard to an acute episode, national guidelines call for high-dose corticosteroids, e.g. oral or intravenous methylprednisolone, neurological evaluation and rehab, and initiation of a course to affect disease progression to possibly include interferon beta, glatiramer acetate, or linoleic acid.
Further, azathioprine, mitoxantrone, intravenous immunoglobulin, plasma exchange, and intermittent courses of high-dose methylprednisolone were designated as appropriate only in designated circumstances.
Finally, anti-viral medications, e.g. acyclovir or tuberculin, cladribine, long-term treatment with corticosteroids, hyperbaric oxygen, linomide, whole-body irradiation, myelin basic protein of any type were designated as not to be used in any circumstances.
Acoustic neuromas can cause facial numbness if their growth impinges on the course of the trigeminal nerve. Usually, a neuroma of this size will also be causing tinnitus and/or vertigo.
Even an inability of sinuses and middle ears to equilibrate barometric pressure has been implicated as a cause for facial numbness.