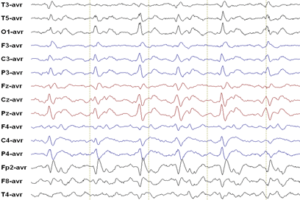
Tremors are the most common movement disorder encountered in clinical practice and can be defined as an involuntary, rhythmic, oscillatory movement of a body part. While tremors predominantly affect the upper extremities (wrist, hands), tremors of the head, lower extremities, and voice can also be encountered.
Classification
Tremors can be broadly classified into rest and action tremors and this differentiation should be the first step in the diagnostic evaluation of a tremor:
- Rest tremors: Occur when the affected body part is at completely relaxed and supported against gravity, for example an arm that is supported by the arm rest. Parkinsonism is the most common etiology of a rest tremor.
- Action tremors: Occur with voluntary contraction of a muscle. Common etiologies of action tremor include essential tremor, enhanced physiologic tremor, drug induced tremor, and cerebellar tremor. Action tremors can be further sub-classified as follows:
- Postural: Occurs when the body part is voluntarily maintained against gravity, for example an outstretched arm.
- Kinetic: Occurs with any form of voluntary movement, for example writing.
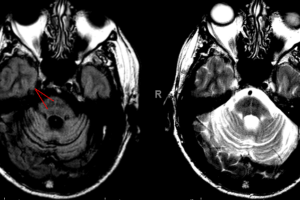
- Intention: Tremor which gets amplified as the target is reached , for example when reaching for an object. This can be elicited with finger-to-nose testing. Intention tremors indicate a cerebellar lesion.
Other historical clues
- Abrupt onset of tremor is more likely to be due to medications, brain tumor, or psychogenic in origin
- Older age at onset is more suggestive of parkinsonism or essential tremor
- Location: Particular causes of tremor preferentially affect certain body parts and therefore the location of the tremor can be an important clue to identifying the cause of the tremor
- Essential tremor is more likely to involve lower extremities, head, and voice
- Parkinsonian tremor is more likely to involve the distal extremities (upper > lower)
Common etiologies of tremor
Enhanced Physiologic tremor
A physiologic tremor is present in all individuals, though is not visible with the naked eye. Certain factors can amplify this physiologic tremor. Frequent causes include alcohol intoxication, alcohol withdrawal, hypoglycemia, anxiety, caffeine intake, thyrotoxicosis.
Medication induced tremor
Medications can be common triggers of tremor. Sympathomimetic drugs (like albuterol, amphetamines, pseudoephedrine) and psychoactive medications (like TCA’s, antipsychotics) are the most likely to exacerbate or induce a new tremor.
Essential tremor
An action tremor that may be bilateral. Family history may be positive as 50% of the cases are transmitted in an autosomal dominant fashion. Patients may note a reduction in the tremor with alcohol consumption and this can be diagnostically helpful.
Parkinsonism
Rest tremor that is generally described as a pill-rolling tremor.
Psychogenic
Abrupt onset (usually after a stressful life event), changing characteristics, and cessation of tremor with distraction suggest a psychogenic etiology.
Diagnostic algorithm for tremor
- Is tremor physiologic? If so, evaluate for causes as listed above.
- Is the patient taking a medication associated with tremor? If so, a trial off the medication is the next step.
- Is the tremor relieved with distraction? If so, evaluate for psychogenic causes.
- If none of the above are present, an evaluation for an organic cause of tremor is warranted.
- Patients younger than age 40 should be screened for Wilson’s disease with a serum ceruloplasmin and 24 hour urinary copper level.
- Patients older than age 40 with a rest tremor are most likely to have parkinsonism and should be evaluated for other symptoms like bradykinesia, rigidity, postural instability.
- Patients older than age 40 (can present earlier as well) with an action tremor are more likely to have essential tremor.
- Patients with an intention tremor should be examined for other cerebellar signs and receive head imaging to rule out stroke, mass, or multiple sclerosis.
Reference
Crawford, Paul. M.D. et al. Differentiation and Diagnosis of Tremor. American Family Physician. March 15, 2011, 83(6):697-702.