Syphilis, a sexually transmitted infection caused by the spirochete Treponema pallidum has recently been re-emerging in the general population. Central nervous system involvement by this infection is referred to as neurosyphilis. Neurosyphilis encompasses a spectrum of CNS manifestations and can present at various times after the initial infection.
Early neurosyphilis can be asymptomatic or present with meningitis, vasculitis, and ocular involvement. Invasion of the CSF by the spirochetes is the first step and probably occurs early after acquisition of the infection.
- Asymptomatic: Some patients remain clinically asymptomatic despite persistent infection of the CSF.
- Meningitis: Symptoms include headache, nausea, vomiting, stiff neck and cranial neuropathies. Seizures can also be the presenting symptom.
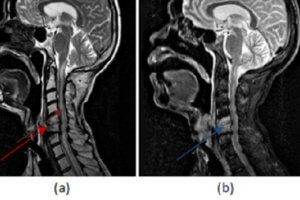
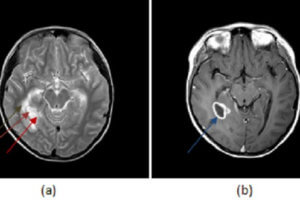
- Vasculitis: An infectious arteritis of the intracranial vessels can develop and may present with focal neurologic symptoms mimicking a stroke. Concomitant syphilitic meningitis is common.
- Ocular: Optic neuropathy, uveitis, and chorioretinitis can be seen with syphilitic involvement of ocular structures
Late neurosyphilis: Clinical manifestations are usually not seen till 10 to 20 years after primary infection and are rarely encountered in the post-antibiotic era.
- General paresis: A form of dementia which starts out with symptoms of forgetfulness and changes in personality and steadily progresses to severe dementia.
- Tabes dorsalis: Affects the posterior columns of the spinal cord resulting in sensory ataxia. Pupillary involvement is also seen. The Argyll-Robertson pupil is the most commonly cited example- a small pupil which does not respond to light, but constricts normally to accommodation and convergence
Diagnosis: The following applies to patients who are negative for HIV. Diagnostic testing in HIV positive patients suspected of having neurosyphilis is slightly different and not discussed here
- For patients with an unknown history of syphilis, diagnostic testing should start with serum serologic tests for syphilis. RPR and VDRL are non-specific screening tests which detect antibodies to antigens that are not entirely unique to Treponema Pallidum. A positive RPR or VDRL should be confirmed with a treponemal specific test like the FTA-ABS (Fluorescent treponemal antibody absorption). RPR and VDRL can be negative in late neurosyphilis and therefore, if suspicion is high, specific testing with the FTA-ABS should be performed even if initial screening tests are negative.
- If a patient has a known history of syphilis or if the serum testing is positive, the next step is evaluation of the CSF. Elevated protein and pleocytosis are usually seen but are non-specific. In contrast to serum studies, a positive CSF VDRL is highly specific for neurosyphilis but not very sensitive. If the CSF VDRL is negative, a CSF FTA-ABS should be ordered. This test is highly sensitive and neurosyphilis is unlikely with a negative CSF FTA-ABS.
Treatment
- Intravenous penicillin G over a 10-14 day course is the standard treatment for neurosyphilis.
Additional Resources and References
Marra, Christina, M.D. Neurosyphilis. Uptodate.com. May 31, 2012