Epidural abscess is a rare condition affecting about 2 in 10,000 patients. Spinal infection typically starts in the disc (discitis), which is seeded through hematogenous dissemination of infection, typically staph aureus and often in drug users.
Diagnosis: Discitis/Osteomyelitis with epidural phlegmon


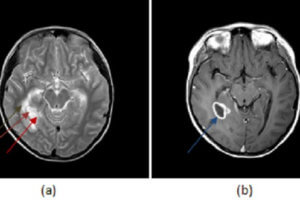
Figure 1: (a, red arrow) T1 sagittal images of the cervical spine demonstrate low T1 signal involving the C5-6 vertebra and replacement of the normal cervical ventral epidural fat signal with low T1 soft tissue (purple arrow). (b, blue arrow) T2 fat saturated images (to cancel out the background fatty marrow signal in the vertebra) show increased T2 signal involving the C5-6 vertebra and disc space most consistent with edema. (c, green arrow) T1 post contrast with fat saturation demonstrates enhancement of the C5-6 vertebra and disc along with enhancement of the ventral epidural space (brown arrow).
Epidural catheter placement is also a risk factor. MR signs of discitis include enhancement and increased T2 signal within the disc space. From there, the infection spreads to the adjacent vertebral body endplates, causing osteomyelitis and suggested by increased T2/STIR signal and enchancement on MR. Infection then spreads into the paravertebral soft tissues, including anterior paraspinal and epidural, as a phlegmon – a mass of high T2, low T1 homogenously enhancing inflammatory cells. As the phelgmon matures central necrosis and fibroblast deposition create an abscess, reflected by lost central but preserved rim enhancement and increased central diffusion restriction. High T2/low T1 signal generally remain, although these signal characteristics can be variable due to the mixture of complex inflammatory debris and necrosis within the abscess. It is important to note mass effect on the adjacent cord or cord signal abnormality since this increases the impetus for acute surgical intervention.
Patients with epidural abscesses and neurological symptoms are generally treated with surgical drainage followed by antibiotics. Those without neurological symptoms will undergo a course of closely supervised antibiotics.