Abscess is in the differential for a rim enhancing mass, an important one in neuroradiology and often remembered by the mnemonic MAGIC DR – metastasis, abscess, glioma, infarct, contusion, demyelination and radiation necrosis.
Diagnosis: Intraparenchymal brain abscess
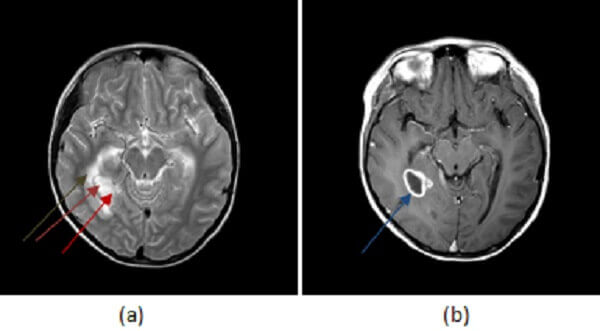
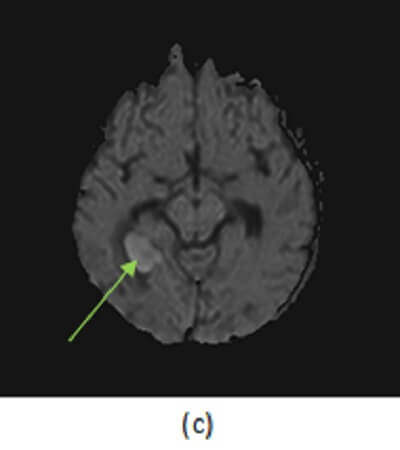
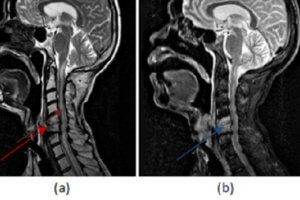
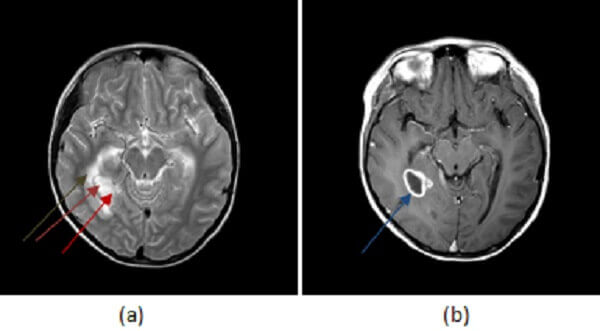
Figure 1: (a) right medial temporal lobe mass has high T2 signal centrally (red arrow) and a low T2 rim (purple arrow). There is surrounding vasogenic edema (brown arrow). (b, blue arrow) T1 post contrast demonstrates thick walled rim enhancement . There is also central restricted diffusion (green arrow, ADC not shown but low signal).
Most brain abscesses result from hematological dissemination of infection; as a result, the grey white junction (site of greatest blood flow) is the most common location. Early infection of the brain parenchyma is termed cerebritis and is characterized by a focal infiltration of inflammatory infiltrates, manifested on MRI by T2/FLAIR hyperintensity without restricted diffusion or enhancement. If left untreated, cerebritis may mature into an abscess – a mass with central necrosis contained by a rim of fibroblasts, manifested by central restricted diffusion with an enhancing, sometimes hypointense T2 rim and extensive vasogenic edema. Smaller “daughter” abscesses may also be present. These characteristics, unique to the pathology of abscesses, help distinguish them from other causes of rim enhancing brain masses.
Brain abscesses are typically treated with antibiotics and drainage, although a conservative approach with antibiotics alone is sometimes considered in patients whose abscesses are located in eloquent cortex or who are poor surgical candidates.