There are many variants on EEG that are considered normal and yet might be confused with epileptiform activity. These benign EEG variants are often found in only certain subpopulations: either young or old patients or patients with specific pathologies that are not epileptogenic. This makes it important to gather at least a basic history of the patient for the proper interpretation of the EEG.
This article adopts the classification of benign EEG (normal) variants as spelled out by Dr Barbara Westmoreland in her chapter entitled “Benign electroencephalographic variants and patterns of uncertain clinical significance” in the classic EEG text edited by Dr. John Ebersole and Dr. Timothy Pedley “Current practice of clinical electroencephalography.”
Each benign EEG variant will be characterized by the population in which it is found, the location at which it is most prominent, the appearance or frequency of events, and the sleep or wake state in which it is found.
Rhythmic, non-epileptiform, benign EEG variants
Rhythmic temporal theta bursts of drowsiness – the most commonly mistaken benign EEG pattern
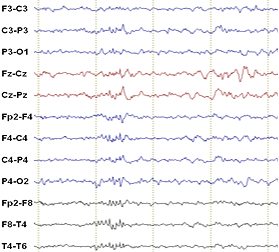
Also called rhythmic midtemporal theta discharges (RMTTD) or psychomotor variant, this bursting pattern occurs during the relaxed awake state or stage I sleep typically in adolescents and young adults. As the name implies, these are runs of sharp, sometimes notched spikes most positive over midtemporal regions. There can sometimes be a waxing-waning pattern to the train of spikes. The trains consist of 5-7 spikes per second and can last for several seconds.
Alpha variants
Alpha activity can present at sub-harmonic frequencies (4-5 Hz, “slow alpha”) or higher harmonics (16-20 Hz, “fast alpha”) of normal alpha activity. Slow alpha is similar to RMTD in spike shape, but are lower in frequency. Both slow and fast alpha are found in occipital or parietal leads since they predominate over the posterior aspect of the head, and both are found in awake adults.
The “alpha squeak” is a high frequency alpha burst (over occipital leads) for 1-2 seconds after an eye blink. Background frequency should not be calculated immediately after a blink due to the alpha squeak.
Mu Rhythm
The mu rhythm is simply alpha-range activity produced by motor and somatosensory cortex that is maximal over central leads. While occipital alpha activity is suppressed by eye-opening, mu activity is suppressed by touch, movement, or movement planning.
SREDA – Subclinical Rhythmic Electrographic (theta) Discharge in Adults
Found in patients over 50, SREDA consists of a train of spiking activity that increases in frequency from 1-2 isolated spikes to 5-7 Hz activity lasting from tens of seconds to minutes. Unlikely epileptogenic activity, SREDA characteristically has an abrupt onset and abrupt offset. This activity can be either unilateral or bilateral, and is typically maximal in the temporo-parietal areas. The proposed etiology is possible subclinical ischemia in watershed zones since the rhythm is found in older patients and the localization correlates with watershed zones.
Midline Theta Rhythm
Midline theta rhythm is a theta-band spike train usually maximal over Cz that is found in both children and adults in the resting awake or stage I sleep states.
Frontal Arousal Rhythm
Frontal Arousal Rhythm (or FAR) is a pattern seen in frontal leads in children soon after awakening or sometimes during light sleep. The frequency of the arousal rhythm is variable, ranging from 7 to 20 Hz. This rhythm dissipates as the child fully wakens.
Paroxysmal hypnogogic hypersynchrony
This is a high amplitude, generalized slowing that presents as 2-3 Hz delta-activity across most or all leads. It is a benign EEG pattern often found in children as they are falling asleep.
Epileptiform but benign EEG variants
Fourteen- and Six-Hertz Positive Bursts
More frequently found in children than adults, these are trains of narrow, positive spikes at either 6-Hz or 14-Hz (14-Hz is more common). They occur during stage I sleep and can be either unilateral or bilateral, most commonly over posterior temporal regions.
Small Sharp Spikes
Small sharp spikes, sometimes called benign epileptiform transients of sleep or BETS, are found during sleep in adults. The morphology is consistent with their name: small (less than 50 microVolts), brief (less than 50 ms), unilateral, mono- or di-phasic spikes usually in the temporal area. They can have a slow-wave that follows the spike, but the slow wave is not typically as large as that of an interictal spike.
SSS 50/50 rule: less than 50 microVolts in amplitude, shorter than 50 ms in duration.
SSS can be differentiated from interictal spikes or epileptogenic discharges because 1) they are isolated, not in trains, 2) they get smaller in slow-wave sleep, 3) they do not have associated slow-wave rhythmic activity, and 4) they are not large enough to distort the background activity. Additional details about their polarity and more subtle morphology can be found in Westmoreland’s chapter (see reference).
Recent studies, however, suggest that some small sharp spikes could in fact be associated with hippocampal epileptiform discharges.
Phantom Spike and Wave (Six-Hertz Spike and Wave Bursts)
This variant appears as a waxing-waning burst of ~6 Hz sinusoidal activity, with a duration of 1-4 seconds. Each sinusoid is the slow-wave component (50-100 microVolts in amplitude) and is preceded by a small, sometimes imperceptable, spike (less than 25 microVolts) – hence the “phantom spike” nomenclature. The activity can be diffuse, found bilaterally and in both anterior and posterior leads. It is found in adolescent and adult patients typically during relaxed wakefulness and stage I sleep.
Wicket Spikes
Apparently first described by an Englishman who knows what a wicket is, these are sharp, tall (60-200 microVolts) spikes that can be found singly or in trains (6-11 Hz) in the temporal areas. The spikes are monophasic (not crossing baseline) with symmetric upsloping and downsloping sides. They are not followed by a wave which helps distinguish them from epileptogenic spikes. Wickets can be found in about 1% of normal patients older than 30.
Breach Rhythm
A breach rhythm is found in patients with a skull defect. Because the skull is missing, normal activity has a larger amplitude in leads over the defect. In addition, waveforms appear sharper despite having a predominant frequency in the theta to alpha range.
References
B Westmoreland (2003) Benign electroencephalographic variants and patterns of uncertain clinical significance in Current practice of clinical electroencephalography edited by Dr. John Ebersole and Dr. Timothy Pedley.
